In 2009, China announced an ambitious health reform aiming to achieve affordable and equitable access to quality basic health care for all by 2020. Between 2009 and 2012, government spending on health care doubled and has since continued to increase. However, money does not necessarily equate to quality service. The fundamental question faced by the government is: how to transform financial resources into effective health care?
In rural China, a three-tiered system with village health posts and township health centers at the base and county hospitals at the top form the cornerstone of health service delivery, serving over 700 million of China’s rural population. Although in theory the three-tiered system is an integrated network of providers; in practice, delivery is fragmented. There is no gatekeeping or care coordination. Different levels of providers compete for patients to maximize revenue and resources are concentrated at the top. There are widespread inefficiencies and quality is in general low and highly variable. Consequently, patients face high and rapidly increasing health care costs while value for money is questionable.
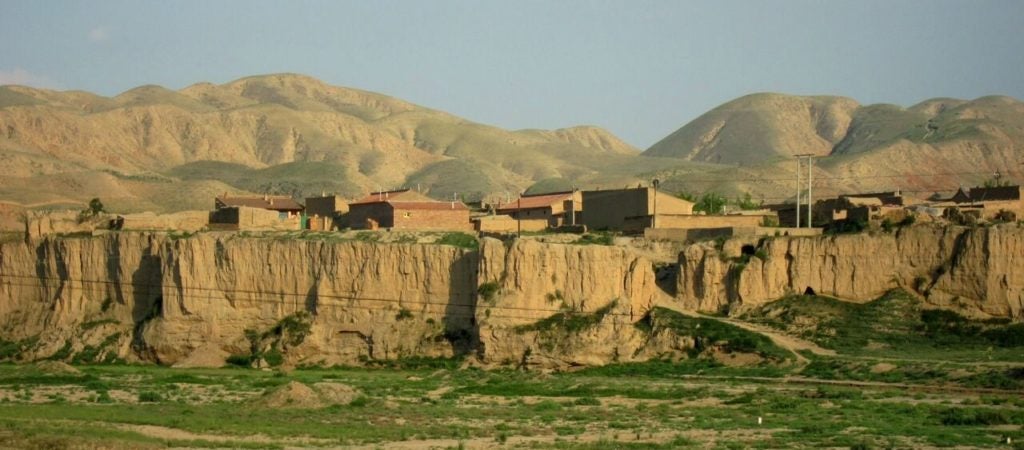
In collaboration with the Government of Ningxia (a low-income province in the northwest of China with 6.3 million people), we launched a social experiment in the province in 2009. The goal is to improve the effective use of resources by establishing a functioning three-tiered delivery system with proper gatekeeping. To that end, a number of policy interventions were designed, implemented and evaluated. They include:
- Changing provider payment for basic health care provided by primary care providers from fee-for-service (FFS) to capitation plus pay-for-performance, with township health centers acting as budget holders that are held accountable for the delivery and quality of both their own services and the services of village health posts under their supervision;
- Changing provider payment for hospital care from FFS to a population-based and disease-adjusted prospective budget plus pay-for-quality, with county hospitals acting as gatekeepers responsible for referrals of complicated cases to above-county tertiary hospitals;
- Re-designing the rural insurance (New Cooperative Medical Scheme—NCMS) benefit package with a tiered copayment structure, to align with the reformed supply-side incentives, to incentivize patients to use primary health care and to seek referrals from county hospitals for specialist hospital services; and
- Shifting tuberculosis (TB) control and treatment from a traditional vertical to a diagonal approach that is integrated within the health system.
For more information see the Policy Intervention page.
The social experiment is a six-year project from 2009 to 2015. It takes place in five counties in Ningxia province, supported by longitudinal household and facility data collection and an electronic management information system (for more information see the Study Design page).
The project has already achieved major policy impact. Within Ningxia, the provincial government has decided to roll out our model to the whole province. At the national level, our model has been identified as a priority rural health system model for the whole nation to emulate (for more information see the Policy Impact and Media Coverage page). A project dissemination conference with participation from national leaders and international and domestic experts was held in May 2014 (for more information see the Conference and Presentations page).
Impact
Based on findings from this pilot study on provider payments, the Ningxia Provincial government decided to scale up project’s interventions from two counties and twenty-eight towns (covering about 0.6 million population) to the whole province. The provider payment interventions have been recognized by the National Family Planning and Health Commission (of China) as innovative and feasible for other rural areas of the nation to emulate. In January 2017, Yanchi County in Ningxia Province was selected as one of the 40 most innovative and impactful reform models in 2016. The project has been further identified as a key model for the nation’s county hospital reform to learn from. The project’s experience has been used as training material for the national county-hospital pilot sites.
Partnership
This project was a collaborative partnership between the University of Oxford, Harvard School of Public Health, Fudan University, Beijing University and Ningxia Medical University (for more information see the Collaborating Partners page). Financial support was provided by the Bill and Melinda Gates Foundation.